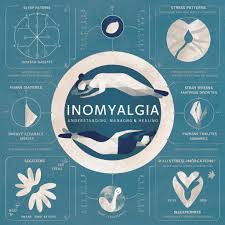
Inomyalgia, commonly understood as a type of muscle pain or discomfort, is a condition that affects millions of individuals worldwide. Muscle pain, or myalgia, can range from mild discomfort to severe, debilitating pain that interferes with daily activities. The term “inomyalgia” often refers to pain associated with specific muscles or systemic conditions that affect muscular function. Understanding inomyalgia is crucial because it can indicate underlying medical issues, ranging from simple overuse or injury to more complex disorders such as fibromyalgia, autoimmune diseases, or metabolic abnormalities. This article explores the causes, symptoms, diagnostic approaches, treatment strategies, lifestyle interventions, and emerging research surrounding inomyalgia, providing a detailed resource for patients, caregivers, and healthcare professionals.
1. What is Inomyalgia?
Inomyalgia is characterized by persistent or recurrent muscle pain that may affect localized areas or multiple muscle groups simultaneously. Unlike temporary muscle soreness from physical exertion, inomyalgia often persists beyond the usual recovery period and may be accompanied by stiffness, tenderness, or weakness. The condition can be acute, developing suddenly due to injury, or chronic, developing over weeks, months, or even years. Chronic inomyalgia often indicates underlying medical conditions or lifestyle factors that exacerbate muscle strain. Understanding the distinction between acute and chronic muscle pain is critical for effective diagnosis and management.
2. Common Causes of Inomyalgia
2.1 Muscle Overuse and Physical Strain
The most common cause of inomyalgia is overuse or strain of the muscles during physical activity, exercise, or repetitive tasks. Activities such as weightlifting, prolonged standing, or improper ergonomics can lead to micro-tears in muscle fibers, causing pain and inflammation. Inomyalgia resulting from overuse is usually localized and improves with rest, hydration, and proper stretching techniques.
2.2 Trauma and Injury
Direct trauma, such as falls, collisions, or heavy lifting, can cause inomyalgia by injuring muscles, tendons, or surrounding soft tissue. Muscle contusions, strains, and minor tears contribute to pain and swelling, often requiring targeted therapy for recovery. Severe injuries may necessitate medical intervention, including imaging studies, physiotherapy, or surgical repair.
2.3 Inflammatory and Autoimmune Conditions
Certain systemic diseases, such as polymyositis, dermatomyositis, and rheumatoid arthritis, can trigger inomyalgia by causing inflammation in muscles and connective tissues. These conditions are often accompanied by fatigue, swelling, or systemic symptoms and require medical evaluation for diagnosis and treatment.
2.4 Metabolic and Endocrine Disorders
Metabolic imbalances, including thyroid dysfunction, vitamin deficiencies, or electrolyte disturbances, can lead to muscle pain. Hypothyroidism, for example, often presents with generalized muscle aches and stiffness. Correcting these imbalances through medical management can alleviate symptoms of inomyalgia.
2.5 Fibromyalgia and Chronic Pain Syndromes
Fibromyalgia is a chronic pain syndrome characterized by widespread musculoskeletal pain, fatigue, and tender points. Patients with fibromyalgia may experience inomyalgia as a persistent symptom that affects quality of life. Management focuses on pain relief, exercise, stress reduction, and multidisciplinary care.
3. Symptoms of Inomyalgia
Symptoms of inomyalgia vary depending on the underlying cause, location, and severity of muscle involvement. Common symptoms include:
-
Persistent or recurrent muscle pain that may worsen with activity
-
Stiffness, tightness, or difficulty moving affected muscles
-
Tenderness to touch or palpation
-
Muscle fatigue or weakness
-
Swelling or inflammation in the affected areas
-
Associated systemic symptoms in cases of autoimmune or metabolic causes, such as fever, weight changes, or fatigue
Recognizing the pattern, intensity, and distribution of symptoms is essential for accurate diagnosis and differentiation from other musculoskeletal or systemic disorders.
4. Diagnosing Inomyalgia
Diagnosis of inomyalgia involves a combination of clinical assessment, medical history, and diagnostic testing. Healthcare professionals may use the following approaches:
-
Physical Examination: Evaluating muscle strength, tenderness, range of motion, and posture.
-
Medical History: Identifying recent injuries, physical activity patterns, family history, and systemic symptoms.
-
Laboratory Tests: Blood tests to detect markers of inflammation, autoimmune activity, or metabolic imbalances.
-
Imaging Studies: MRI, ultrasound, or X-rays to assess structural abnormalities, tears, or inflammation in muscles.
-
Specialized Tests: Electromyography (EMG) or nerve conduction studies for suspected neuromuscular involvement.
An accurate diagnosis is critical for effective treatment, as inomyalgia can be a symptom of multiple underlying conditions.
5. Treatment and Management Strategies
5.1 Medication
Depending on the cause, medications may include:
-
Analgesics for pain relief (acetaminophen or NSAIDs)
-
Muscle relaxants for spasms or tension
-
Corticosteroids for inflammatory conditions
-
Disease-modifying drugs for autoimmune causes
5.2 Physical Therapy and Exercise
Targeted physical therapy helps strengthen muscles, improve flexibility, and reduce pain. Low-impact exercises such as swimming, yoga, and stretching routines are beneficial for chronic inomyalgia.
5.3 Lifestyle Interventions
Lifestyle modifications play a key role in managing muscle pain:
-
Balanced diet rich in vitamins, minerals, and protein
-
Adequate hydration to maintain muscle function
-
Stress management techniques, including mindfulness, meditation, and adequate sleep
-
Ergonomic adjustments to reduce repetitive strain
5.4 Complementary Therapies
Some patients find relief through massage therapy, acupuncture, heat or cold therapy, and relaxation techniques. Integrating these methods with conventional treatment can enhance outcomes.
6. Preventing Inomyalgia
Prevention focuses on reducing risk factors and promoting muscle health:
-
Gradual progression of exercise intensity
-
Proper warm-up and cool-down routines
-
Maintaining good posture and ergonomic habits
-
Adequate rest and recovery periods for muscles
-
Regular medical checkups to detect underlying conditions early
Preventive strategies are especially important for athletes, manual laborers, and individuals with predisposing conditions.
7. Emerging Research and Future Directions
Current research explores the underlying mechanisms of chronic muscle pain, including nerve-muscle interactions, genetic predisposition, and inflammatory pathways. Advances in regenerative medicine, targeted drug therapy, and personalized physiotherapy approaches promise to improve the management of inomyalgia in the coming years. Additionally, digital health solutions, wearable technology, and telemedicine offer new tools for monitoring symptoms, guiding rehabilitation, and enhancing patient engagement.
FAQs
Q1: How long does inomyalgia last?
Duration depends on the underlying cause; acute cases may resolve in days or weeks, while chronic cases can persist for months or years.
Q2: Can stress cause inomyalgia?
Yes, chronic stress can contribute to muscle tension, pain, and fatigue, exacerbating inomyalgia symptoms.
Q3: Are there home remedies for mild inomyalgia?
Rest, gentle stretching, heat/cold therapy, hydration, and over-the-counter pain relievers can alleviate mild muscle pain.
Q4: When should I see a doctor for muscle pain?
Seek medical attention if pain is severe, persistent, associated with swelling or weakness, or accompanied by systemic symptoms.
Q5: Can exercise help with chronic inomyalgia?
Yes, low-impact exercises, physical therapy, and targeted strengthening routines can reduce pain, improve flexibility, and enhance muscle function.
Conclusion
Inomyalgia, characterized by persistent or recurrent muscle pain, affects individuals differently depending on underlying causes, lifestyle factors, and health conditions. Proper diagnosis, tailored treatment, lifestyle modifications, and preventive strategies are essential for managing symptoms and improving quality of life. Emerging research and modern therapies continue to enhance our understanding and management of this condition, offering hope for more effective, personalized interventions. Awareness, early detection, and proactive management remain key to addressing inomyalgia safely and effectively.