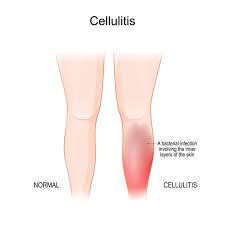
Cellulitis is a common but potentially serious bacterial skin infection that affects millions of people worldwide each year. It occurs when bacteria, most often Streptococcus or Staphylococcus species, penetrate the skin through cuts, abrasions, or other breaks in the protective barrier, leading to inflammation, redness, swelling, and pain. While cellulitis can occur in anyone, certain groups—such as the elderly, individuals with weakened immune systems, or those with chronic skin conditions—are at higher risk. The infection can progress rapidly if left untreated, sometimes leading to severe complications like sepsis or deep tissue infection. This article explores cellulitis in depth, covering its causes, symptoms, diagnosis, treatment, prevention, complications, and current medical research, providing a comprehensive understanding for both patients and healthcare providers.
1. Causes of Cellulitis
Cellulitis primarily results from bacterial infections, most commonly Streptococcus pyogenes and Staphylococcus aureus, including MRSA (methicillin-resistant Staphylococcus aureus). The infection occurs when bacteria enter the skin through open wounds, insect bites, surgical incisions, burns, or even minor abrasions. Individuals with compromised skin integrity, chronic edema, diabetes, or immune deficiencies are more susceptible. Factors such as poor circulation, obesity, and lymphedema further increase risk. Understanding the causes of cellulitis is crucial because it highlights the importance of skin care, hygiene, and early treatment to prevent infections from escalating into severe conditions.
2. Risk Factors
Certain populations are more vulnerable to developing cellulitis. Risk factors include:
-
Chronic conditions: Diabetes, vascular disease, or immune system disorders weaken the body’s defenses.
-
Skin injuries: Cuts, scrapes, burns, insect bites, surgical wounds, or eczema compromise the skin barrier.
-
Obesity: Excess weight can contribute to poor circulation and skin folds, promoting bacterial growth.
-
Edema and lymphedema: Fluid accumulation in limbs can make the skin more prone to infection.
-
Weakened immunity: Elderly individuals or those on immunosuppressive medications are at higher risk.
By understanding these risk factors, patients and healthcare providers can take preventive measures to minimize the likelihood of infection.
3. Symptoms and Signs
Cellulitis typically presents with localized redness, swelling, warmth, and tenderness of the affected area. The skin may appear shiny or tight, and in some cases, blisters or pus-filled lesions can form. Patients often experience fever, chills, fatigue, and malaise as the infection progresses. The severity of symptoms can vary depending on the location and depth of infection, the type of bacteria involved, and the patient’s overall health. Recognizing early signs is essential because prompt medical intervention can prevent complications and limit the spread of bacteria to deeper tissues or the bloodstream.
4. Diagnosis and Medical Evaluation
Diagnosis of cellulitis primarily involves a clinical evaluation by a healthcare professional. Physicians typically assess the affected area, review patient history, and identify risk factors. Blood tests, wound cultures, or imaging studies such as ultrasound or MRI may be used in severe or atypical cases to confirm the infection or rule out abscesses and deep tissue involvement. Misdiagnosis is common because cellulitis can mimic other conditions like eczema, deep vein thrombosis, or allergic reactions. Accurate diagnosis ensures timely treatment and reduces the risk of serious complications.
5. Treatment Approaches
Treatment of cellulitis usually involves antibiotics to eradicate the bacterial infection. The choice of antibiotic depends on the severity of infection and whether MRSA is suspected. Mild cases can often be treated with oral antibiotics, while severe cases may require intravenous therapy in a hospital setting. Pain relief, elevation of the affected limb, and supportive care such as hydration and rest are also important components of treatment. In rare cases, surgical intervention may be necessary to drain abscesses or remove infected tissue. Prompt treatment is crucial to prevent progression to systemic infection or chronic skin damage.
6. Complications of Cellulitis
If left untreated or inadequately managed, cellulitis can lead to serious complications. Potential complications include:
-
Sepsis: When bacteria enter the bloodstream, leading to a life-threatening systemic infection.
-
Lymphangitis: Infection of the lymphatic vessels that can cause spreading inflammation.
-
Chronic swelling: Recurrent cellulitis can result in lymphedema or permanent tissue changes.
-
Abscess formation: Collection of pus that may require surgical drainage.
Awareness of these potential outcomes underscores the importance of early diagnosis, adherence to prescribed treatment, and regular monitoring.
7. Prevention Strategies
Preventing cellulitis involves protecting the skin, maintaining good hygiene, and managing risk factors. Key preventive strategies include:
-
Keeping wounds clean, covered, and properly dressed.
-
Moisturizing dry skin to prevent cracks or fissures.
-
Managing chronic conditions such as diabetes and vascular disease.
-
Avoiding scratches or bites from pets and insects.
-
Using compression therapy or exercises for patients with lymphedema or chronic swelling.
Education on prevention is vital for at-risk individuals to reduce recurrence and limit healthcare complications.
8. Cellulitis in Special Populations
Certain groups require specialized attention:
-
Children: Skin infections may occur after cuts, insect bites, or chickenpox lesions, requiring careful monitoring.
-
Elderly: Reduced immunity and comorbidities make cellulitis more severe in older adults.
-
Diabetic patients: Neuropathy and poor circulation can mask early symptoms, leading to delayed diagnosis.
-
Immunocompromised patients: Patients with chemotherapy, HIV, or long-term steroid use are at higher risk of severe infection.
Tailoring management approaches to these populations ensures effective treatment and reduces complications.
9. Advances in Research and Treatment
Ongoing research focuses on understanding bacterial resistance, improving diagnostic tools, and developing new antibiotics or topical treatments. Studies also explore adjunct therapies such as probiotics, immunomodulation, and novel wound care technologies to accelerate healing and prevent recurrence. Telemedicine and remote monitoring have emerged as effective tools for early evaluation and follow-up, particularly in rural or underserved areas. Keeping abreast of these advancements helps clinicians provide evidence-based care and improve patient outcomes.
10. When to Seek Medical Attention
Immediate medical attention is warranted if cellulitis shows:
-
Rapidly spreading redness or swelling.
-
Fever, chills, or systemic symptoms.
-
Pain, numbness, or discoloration of the affected area.
-
Non-healing wounds or recurrent infections.
Early intervention reduces the risk of complications, prevents hospitalization, and ensures faster recovery.
FAQs
1. What causes cellulitis?
Cellulitis is caused by bacteria, most commonly Streptococcus or Staphylococcus, entering the skin through cuts, abrasions, or other breaches.
2. Can cellulitis spread from person to person?
No, cellulitis is generally not contagious; it results from bacteria entering compromised skin.
3. How is cellulitis treated?
Treatment usually involves oral or intravenous antibiotics, pain management, and supportive care such as rest and limb elevation.
4. How long does it take to recover?
Mild cellulitis may improve within a few days of antibiotics, while severe cases may take several weeks to fully heal.
5. Can cellulitis recur?
Yes, individuals with risk factors such as diabetes, chronic edema, or repeated skin injuries may experience recurrent infections.
Conclusion
Cellulitis is a common but potentially serious bacterial skin infection that requires prompt recognition, accurate diagnosis, and timely treatment. Understanding the causes, risk factors, symptoms, and complications is essential for preventing severe outcomes. Effective management involves antibiotics, supportive care, and lifestyle modifications to reduce recurrence risk. Advances in medical research, patient education, and preventive strategies continue to improve outcomes for individuals affected by cellulitis. By prioritizing early intervention, risk management, and proper skin care, patients can successfully navigate this condition while minimizing complications and ensuring long-term skin health.